Abstract
Introduction: Mantle cell lymphoma (MCL) is a CD5+ B-cell lymphoma characterized by cyclin D1 expression. The disease has heterogeneous clinical outcomes: in a subset of patients, it is indolent but many others have an aggressive course with poor outcome. Consolidative autologous hematopoietic cell transplant (HCT) in 1st remission is often employed for fit patients ≤65; however the benefit of this approach remains uncertain without prospective validation in the rituximab era. Herein we retrospectively assessed the impact of HCT consolidation following induction therapy on survival in a large multicenter cohort of transplant eligible patients aged ≤65.
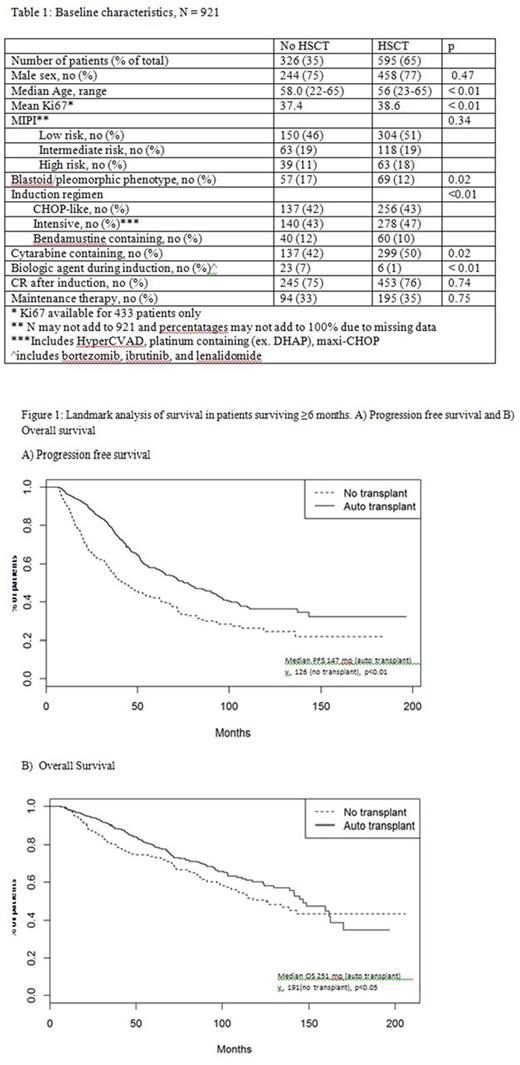
Methods: We retrospectively studied adults with newly diagnosed MCL, aged ≤65, transplant eligible at diagnosis, and treated with induction chemotherapy from 2000-2015. Eligibility for transplant was determined by the institutional chart reviewer. 22 US and Canadian academic medical centers contributed. Information on prognostic markers, treatment, response to induction, and survival was collected. The primary objective was to assess for an overall survival (OS) benefit of HCT consolidation in first remission. A landmark survival analysis was restricted to patients surviving >6 months who achieved ≥partial response (PR) after induction, with OS and progression-free survival (PFS) defined as time from diagnosis to event (death or relapse). Cox multivariate regressions were performed to evaluate the effect of HCT consolidation on OS and PFS after adjusting for confounders (age, sex, MIPI, stage, induction regimen, blastoid/pleomorphic phenotype, response to induction (complete response (CR) vs. PR), and maintenance therapy. Due to the differential times of HCT, this was included in the model as a time-varying covariate. Ki67 was excluded from regression models as it was available in <50% of patients.
Results: Data was collected for 1113 patients, and 921 patients met inclusion criteria. HCT was performed in 595 patients (64%). The two most common reasons for not performing HCT were physician (46%) or patient preference (23%). Three centers, who contributed a combined 135 patients, performed HCT in < 50% of eligible patients. Median time from diagnosis to HCT was 7 months. Patients who received consolidative HCT were younger, less likely to have blastoid or pleomorphic morphology, more likely to have received an intensive regimen (e.g. HyperCVAD +/- cytarabine, platinum containing, or maxi-CHOP) and cytarabine, and less likely to have received biological agents (bortezomib, lenalidomide, and ibrutinib) during induction (table 1). Median follow-up for the cohort was 78.1 months (6.5 years), with median PFS of 62.9 months (5.2 years) and OS of 141.5 months (11.7 years). On unadjusted landmark analysis, HCT in 1st remission was associated with improved PFS (p<0.01) (Figure 1A) and improved OS (p=0.03) (Figure 1B). On multivariate analysis, this association persisted, with HCT resulting in improved PFS (HR 0.57, 95%CI 0.47-0.70, p<0.01) and OS (HR 0.73, CI 0.57-0.94, p=0.01). Other variables associated with improved PFS included lower MIPI (HR 0.49, CI 0.36-0.65, p<0.01 for low vs. high MIPI); non-blastoid or pleomorphic morphology (HR 0.60, CI 0.47-0.76, p<0.01); use of an intensive regimen (HR 0.63, CI 0.41-0.98, p=0.04), bendamustine (HR 0.54, CI 0.33-0.89, p=0.01), or biologic agent (HR 0.42, CI 0.20-0.89, p=0.02) during induction; CR with induction (HR=0.51, CI 0.41-0.64, p<0.01); and use of maintenance (HR 0.57, CI 0.45-0.72, p<0.01). Variables associated with improved OS included lower MIPI (HR 0.34, CI 0.24-0.48, p<0.01), non-blastoid or pleomorphic morphology (HR 0.44, CI 0.33-0.58, p<0.01), CR to induction (HR=0.55, CI 0.42-0.72, p<0.01), and use of maintenance (HR 0.61, CI 0.45-0.83, p<0.01). Death within 100 days of transplant occurred in 7 patients (1.2%). 18 patients developed secondary AML or MDS (incidence 2.4% with HCT consolidation (n=14) vs. 1.2% (n=4) without).
Conclusion: In this large cohort of younger transplant eligible patients with MCL, HCT consolidation in first remission was associated with significantly improved OS and PFS after adjusting for prognostic factors and differences in initial treatment. Within the limitations of retrospective analysis and inherent selection bias, our findings support the benefit of HCT consolidation following induction therapy for fit patients ≤65 in the rituximab era.
Barta: Janssen: Membership on an entity's Board of Directors or advisory committees; Seattle Genetics: Research Funding; Merck: Research Funding; Celgene: Membership on an entity's Board of Directors or advisory committees, Research Funding; Takeda: Research Funding. Villa: Roche: Consultancy, Honoraria, Other: Travel, Research Funding; Lundbeck: Consultancy, Honoraria, Other: Travel; Seattle Genetics: Consultancy, Honoraria; Celgene: Consultancy, Honoraria; Amgen: Consultancy, Honoraria; Janssen: Honoraria; Abbvie: Other: Travel. Gerrie: Roche: Research Funding; Seattle Genetics: Honoraria, Membership on an entity's Board of Directors or advisory committees; Lundbeck: Honoraria; Janssen: Membership on an entity's Board of Directors or advisory committees. Fenske: Celgene: Consultancy; Sanofi: Consultancy; Pharmacyclics: Consultancy. Maddocks: Merck: Research Funding; Pharmacylics: Research Funding; BMS: Research Funding; Novartis: Research Funding. Lansigan: Spectrum Pharmaceuticals: Consultancy, Research Funding; Seattle Genetics: Consultancy. Reddy: Abbvie: Consultancy; BMS: Consultancy; Celgene: Consultancy; Gilead: Speakers Bureau. Landsburg: Curis: Consultancy, Research Funding; Takeda: Research Funding. Karmali: Celgene: Speakers Bureau. Kaplan: Takeda: Research Funding; Millennium: Research Funding; Seattle Genetics: Research Funding; Janssen: Research Funding. Caimi: Celgene: Speakers Bureau; Abbvie: Equity Ownership; Seattle Genetics: Equity Ownership; Incyte: Equity Ownership. Cohen: Takada: Research Funding; Bristol Myers Squibb: Research Funding; Abbvie: Consultancy, Membership on an entity's Board of Directors or advisory committees; Janssen: Consultancy, Membership on an entity's Board of Directors or advisory committees; Genentech: Consultancy, Membership on an entity's Board of Directors or advisory committees; Bioinvent: Consultancy, Membership on an entity's Board of Directors or advisory committees; Novartis: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding; LAM Therapeutics, Inc: Research Funding; Infinity: Consultancy, Membership on an entity's Board of Directors or advisory committees. Calzada: Seattle Genetics: Research Funding. Handorf: Pfizer: Research Funding. Bachanova: Seattle-Genetics: Consultancy, Membership on an entity's Board of Directors or advisory committees; Juno: Membership on an entity's Board of Directors or advisory committees; Oxis: Membership on an entity's Board of Directors or advisory committees, Research Funding; Zymogen: Consultancy, Membership on an entity's Board of Directors or advisory committees; Novartis Pharmaceuticals Corporation: Membership on an entity's Board of Directors or advisory committees, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal